A day-in-the-life of NICU Medical Director Dr. Cristina Miller

Hennepin Healthcare is made up of over 7,000 team members who work in a variety of locations and specialties across our system. We’re here for every stage of a patient’s life – including the very beginning. To give you a behind-the-scenes look at this journey, we spent some time in the Neonatal Intensive Care Unit to share a day-in-the life of NICU Medical Director Cristina Miller, MD.
Dr. Miller, a neonatologist, started at Hennepin Healthcare this past December after working at Children’s Hospital for nine years. Dr. Miller had always known she wanted to work in pediatrics and discovered a love for the inpatient setting early on: “I really enjoyed inpatient care and helping families through some of the most difficult hours or days of their life.”
Although the opportunity to work as a medical director was one aspect of Dr. Miller’s desire to come to Hennepin, a small, tight-knit NICU team was also something she was looking for. “Everyone knows each other, really,” says Dr. Miller. “I loved the idea of a smaller unit. Everyone is cohesive and works together here.”
Read on to learn how Dr. Miller and her team work together to care for some of Hennepin Healthcare’s tiniest patients.
8 am – Shift starts in the NICU

The NICU is divided into two main patient areas or “pods.” The first pod holds 12 beds and is intended for sicker patients who require more constant monitoring and care. The second pod, which holds 9 patient beds, is more so intermediate care and holds patients that still need a NICU level of care but are able to breathe on their own and aren’t quite as sick. Although it varies, the average census, or number of patients at one time, in the NICU is 17.
There’s only one physician in the NICU at a time. But that’s only because any provider or specialist can be called over as needed from another area of the hospital. Dr. Miller rotates shifts with three other neonatologists. Along with a team made up of nurses and 6 specialized neonatal nurse practitioners, this is the NICU team.
9 am – Patient rounding

During rounding, Dr. Miller and other members of the team go around to each patient to discuss their past few hours of care and any concerns that have come up. A patient’s family is always asked to participate if they’re in the NICU during rounding. A lactation consultant, medical students, and team members from our Pharmacy and Nutrition teams are also often in attendance, though not every day. “Everyone has something really important and valuable to bring,” says Dr. Miller. “We all have this one common goal: safe, healthy babies.”
The length of time it takes to complete rounding varies, but it usually lasts a few hours. Rounding ensures Dr. Miller is able to hear from all members of her team and know how each patient is progressing.
1 pm – Lunch break
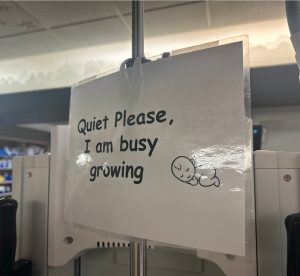
Lunchtime is not only a time to refuel, but also reminds team members why they do the work they do: inside the NICU breakroom is a bulletin board filled with dozens of heartfelt thank you letters and update photos from the families of patients who have graduated from the NICU.
2 pm – Call patient families

Every day, Dr. Miller will call the parents of her NICU patients to give them updates and share what was discussed during rounding. Dr. Miller will often work with our Interpreter Services department on these calls, as it is not uncommon to speak to patient families with limited English proficiency.
3 pm – Meet with nurse manager/administrative work
As part of her work as medical director, Dr. Miller will regularly meet with the nurse manager to go over more of the administrative aspects of her role. This can include tasks such as managing equipment and protocols but also includes patient care quality and keeping up on best practices.
Dr. Miller and her team also have access to data from NICUs across the country which allows her to see how Hennepin Healthcare’s NICU is performing in comparison to other NICUs. This helps guide improvement efforts to ensure the unit is using the latest in evidence-based practices.
4 pm – End of shift
No two days in the NICU are the same, but two things that are always consistent are this team’s passion and expertise.
NICU patients have some of the longest lengths of stay in the hospital. Although they know their child is receiving the best possible care from Dr. Miller and her team, this time is often scary and stressful. A common joke expressed by parents as their baby is discharged from the NICU and is finally able to go home is, “Thanks for everything, but I hope I never see you again.”
As the population grows each year, there is more need for NICU beds. “10-15% of all babies end up needing us. Some are short term, some are months-long,” says Dr. Miller. She hopes that as work continues on Hennepin Healthcare’s Comprehensive Campus Development Plan, the NICU will be able to expand not only to house more patients, but also to give parents and families more space to be with their babies.
“While there are certainly highs and lows in the NICU, our patients are resilient and the majority do incredibly well,” says Dr. Miller. “It is a place in the hospital filled with hope and healing and I am grateful to be a part of that.”

