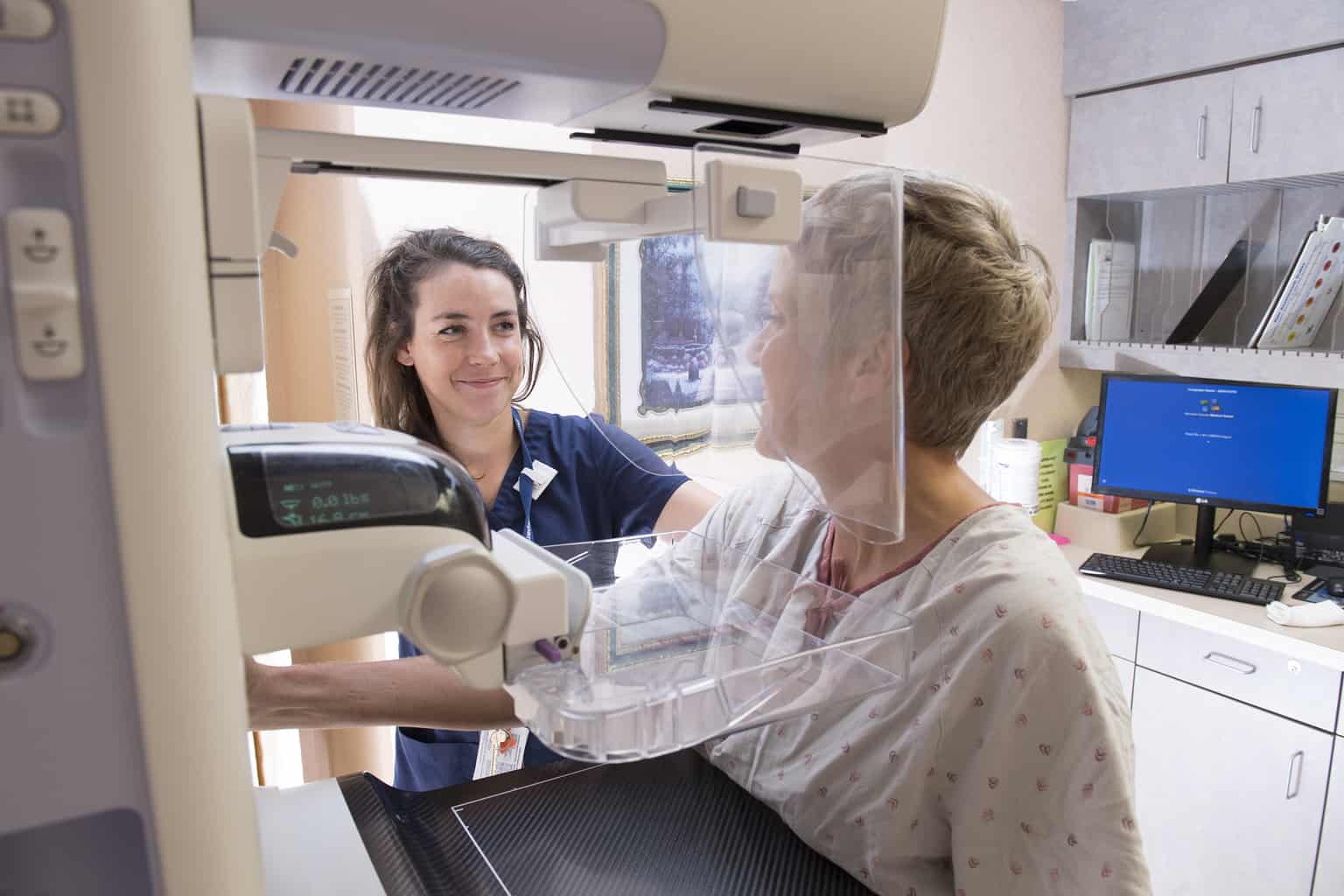
Mammography
Mammography is a very safe procedure that uses low doses of radiation to produce high quality x-rays that help medical professionals identify and prevent breast cancer.
Locations
Mammography and Your Health
Lifesaving strategies get more important as you get older.
Breast cancer often makes itself known in its early stages, when there's a good chance for a cure. But here's the catch: You must be doing the right screenings to detect breast cancer. That includes monthly breast self-exams, regular clinical breast exams, and regular mammograms.
Yet many women still put off these exams for any number of reasons. If you have an excuse for not being tested, read on. The following reasons to get screened should help convince you that now is the time to take action.

Frequently Asked Questions about Mammograms
A screening mammogram usually involves two images of each breast. For some patients, more images may be needed in order to see as much breast tissue as possible.
Diagnostic mammography involves additional views of the breast, and is used when an abnormality is found during a screening mammogram, or in women who have breast complaints or symptoms such as a breast lump, breast pain, or skin irritation.
3D Mammography – locations, benefits
Hennepin Healthcare offers advanced 3D mammography service. 3D mammography is similar to having a conventional mammogram but is proven to be more accurate. Like a traditional mammogram, 3D mammography takes images of your breast from multiple angles but is able to capture multiple images of the breast from several angles. Providers recommended 3D mammography in cases where increased accuracy is needed.
According to the American College of Radiology's Practice Parameter for the Performance of Screening and Diagnostic Mammography, the following are recommended indicators for getting a mammography screening:
- Annually for asymptomatic women age 40 and older who are at average risk for breast cancer.
- Asymptomatic women under age 40 who are at increased risk for breast cancer.
- Woman with known mutation or genetic syndrome with increased breast cancer risk: yearly starting by age 30, but not before age 25.
- Untested women with a first-degree relative with known BRCA mutation: yearly starting by age 30, but not before age 25.
- Women with a 20% or greater lifetime risk for breast cancer based on breast cancer risk models: yearly starting by age 30, but not before 25, or 10 years earlier than the age at which the youngest first-degree relative was diagnosed, whichever is later.
- Women with a history of chest (mantle) radiation received between the ages of 10 and 30: yearly starting 8 years after the radiation therapy, but not before the age 25.
- Woman with biopsy-proven lobular neoplasia, atypical ductal hyperplasia (ADH), ductal carcinoma in-situ (DCIS), invasive breast cancer, or ovarian cancer: yearly from time of diagnosis, regardless of age.
- Age at which annual mammography screening should end.
- There are no defined upper age limit at which mammography may not be beneficial.
- Screening with mammography should be considered as long as the patient is in good health and is willing to undergo additional testing, including biopsy, if an abnormality is detected.
- If you have had mammograms in a different facility, arrange to have your previous mammograms, reports, and any treatment reports forwarded
- Do not wear deodorant, powder or cream under your arms as it may interfere with your mammogram images
- You will be asked to undress above the waist and will be given a gown to wear during your mammogram
- Your mammogram will be read by a radiologist
- A report will be sent to your provider
- A letter will also be sent to you with the result of your mammogram

